"Good enough" provider data quality is costing plans millions they're not tracking.
If you're reading this, your provider data probably isn't broken. It's just... good enough.
Rosters get processed (eventually). Directories get updated (mostly). Members find providers (sometimes). And when problems surface, your team scrambles, fixes them, and moves on.
But here's the uncomfortable truth: "good enough" provider data quality is costing your Medicare Advantage plan millions. You just don't measure data quality like you measure claims accuracy.
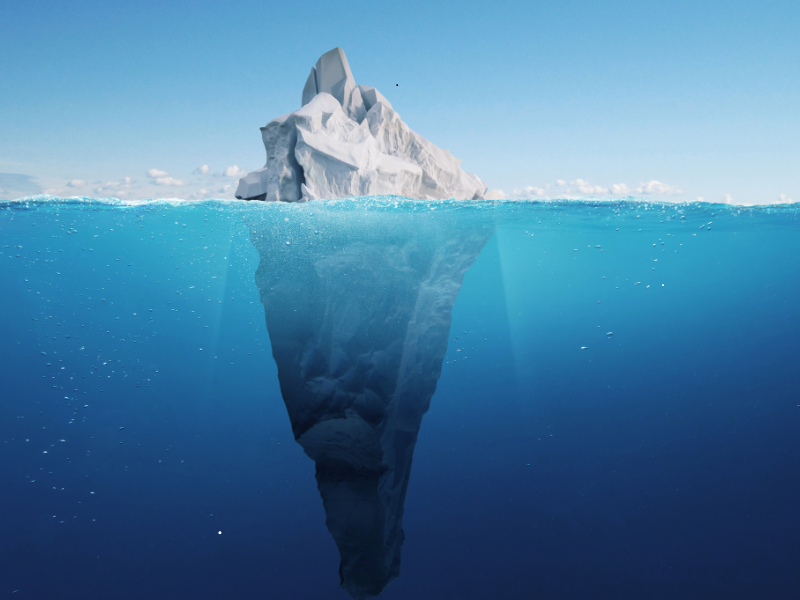
Remember the parable of the frog in boiling water? Drop a frog into a pot of boiling water, and it jumps out immediately. But place it in cool water and gradually heat it up, and the frog doesn't notice the danger until it's too late. (Grim metaphor, we know.)
Your provider data quality challenges work the same way.
An acute crisis, like a CMS audit finding or a class-action lawsuit, gets everyone's attention. Budgets open. Priorities shift. Solutions get implemented.
But chronic pain persists: The weekly roster that takes three days to process manually? The directory complaints that trickle in one by one? The data governance team burning hours reconciling duplicates across systems? That's just "how things work around here."
The problem is that chronic pain adds up faster than acute crises; it's just diffused across enough departments that no single budget owner feels the full weight.
Let's make the invisible visible. Research shows that administrative costs in healthcare are significantly higher than they need to be, with provider data management cited as a major pain point across Medicare Advantage organizations.
Here's where the costs hide:
Provider data management is complex and resource-intensive. Health plans must manage updates every time a physician changes hours, practice location, or credentialing status—and these updates typically happen manually across multiple databases. One industry analysis found that "healthcare’s general and administrative expenses as a percent of revenues are nearly double those of other industries" 1 . Payers need comprehensive provider data management systems to track and manage information, as manual processes significantly slow operations and create accuracy risks.
The credentialing process alone is notoriously burdensome: physicians often spend over five months waiting to be credentialed with a payer, while payers must manually process applications submitted in various formats.2 Building tools that allow for automatic intake and real-time updates of provider information can save substantial time and improve data accuracy.
For context: providers caring for patients in certain Florida zip codes may need to manage contracts with up to 47 concurrent Medicare Advantage plans, each with unique payment models and documentation requirements.3 This complexity forces providers to develop separate collection strategies for each payer, creating crossfire that drives up administrative costs for both sides.
Healthcare contact centers handle significant call volume related to provider directory issues. Industry data shows that the average cost per call in healthcare contact centers is approximately $4.90,4 with some sources citing costs in the $8-12 range depending on complexity and handle time.
When members encounter incorrect phone numbers, office closures, or outdated provider affiliations in directories, it damages trust in the health plan. Studies indicate that 42% of patients identify difficulty in reaching their provider as the largest barrier to good healthcare communication.5 Directory-related complaints generate call volume that could be prevented with better data quality, and these calls often require longer handle times as agents work to find correct information.
The regulatory stakes are high and getting higher. CMS conducted phone surveys of Medicare Advantage provider directories between 2017-2018 and found that over 48% of locations listed for primary care, cardiology, oncology, or ophthalmology providers had at least one inaccuracy in terms of address, phone number, or whether the provider accepted new patients.6
CMS has strengthened enforcement in response to these findings. Medicare Advantage organizations now face:
In 2024 alone, CMS imposed civil monetary penalties totaling over $1 million on 16 sponsors for 23 violations, with the largest single penalty reaching $2 million.10 While these specific penalties weren't all directory-related, they demonstrate CMS's increasingly aggressive audit and enforcement posture.
Member experience scores suffer when provider search frustrates members. When directories are inaccurate, members may unknowingly see out-of-network providers, triggering unexpected charges and complaints. This directly impacts CAHPS measures and overall member satisfaction—which in turn affects Star ratings and revenue.
Organizations often build workaround systems and shadow databases to compensate for master data gaps. Data inaccuracies cause claim denials and rework when NPIs are incorrect, licenses are outdated, or information doesn't match across systems.11 These operational inefficiencies compound over time.
When you add up the diffused costs across these departments—manual processing time, call center overhead, compliance response, audit preparation, claims rework, and quality impact—"good enough" provider data quality represents a multi-million dollar annual cost for most Medicare Advantage plans. And that's before any major compliance event.
Most plans don't measure these diffused costs—until something forces them to pay attention:
When CMS reviews find that nearly half of provider locations have inaccuracies, the consequences extend beyond immediate corrective action. Plans must document data quality processes, demonstrate remediation, and prepare for ongoing scrutiny.
A half-star drop in CAHPS measures tied to access and member experience can cost plans millions in lost revenue. When root cause analysis points back to provider search frustration and directory accuracy, that's an expensive wakeup call.
Provider or member class actions alleging directory inaccuracy can cost millions in legal fees and settlements—not to mention reputation damage and increased regulatory scrutiny.
Acquiring another plan sounds great until you try to merge provider data and discover duplicate NPIs, conflicting specialties, and no clear source of truth across systems.
Want to expand into a new county or add a new product line? "Good enough" provider data governance will slow you down exactly when speed to market matters most.
Here's the mindset shift that transforms provider data from a cost center to a strategic asset:
Stop treating provider data like facilities management (something that only matters when it breaks) and start treating it like claims accuracy (something you measure, monitor, and optimize continuously).
Ask yourself:
If you don't have crisp answers to these questions, you're flying blind—and almost certainly overpaying for "good enough."
The Medicare Advantage plans that have solved this challenge share three characteristics:
These plans aren't accepting "good enough" anymore. They're achieving:
In Part 2 of this series, we'll tackle the objection we hear most often—and the one that keeps more plans stuck than any other: 'Our data is too messy for AI to handle.'
Spoiler: That's exactly backwards.
But if you're reading this and thinking, "We need to measure what 'good enough' is actually costing us," let's talk.
Book a 15-minute call to see CareLoaDr process your actual roster in real time—and what that could mean for your team's time, your member experience, and your compliance posture.
Leap Orbit builds provider data infrastructure for Medicare Advantage plans. Our modular Convergent platform, CareLoaDr AI, and CareFinDr solutions help plans turn messy, fragmented provider data into a strategic asset, without the enterprise price tag or implementation timeline.
Last reviewed: October 2025
Footnotes